Knee Arthroscopy
Knee arthroscopy is a minimally invasive surgical procedure used to diagnose and treat problems within the knee joint. During the procedure, a small camera called an arthroscope is inserted into the knee through a small incision, allowing the surgeon to view the inside of the joint on a screen. Overall, knee arthroscopy is a less invasive option that offers quicker recovery and less post-operative pain compared to traditional knee surgeries.
Who needs knee arthroscopy?
If you have knee pain that doesn’t get better with nonsurgical treatments (rest, ice, nonsteroidal anti-inflammatory drugs and physiotherapy). Although arthritis causes knee pain, arthroscopic knee surgery isn’t always an effective treatment for osteoarthritis.
What conditions does knee arthroscopy treat?
- Meniscus tears
- Ligament injuries (e.g., ACL tears)
- Patella problems (e.g., patellar tracking disorder)
- Cartilage damage
- Inflammation or infection in the joint
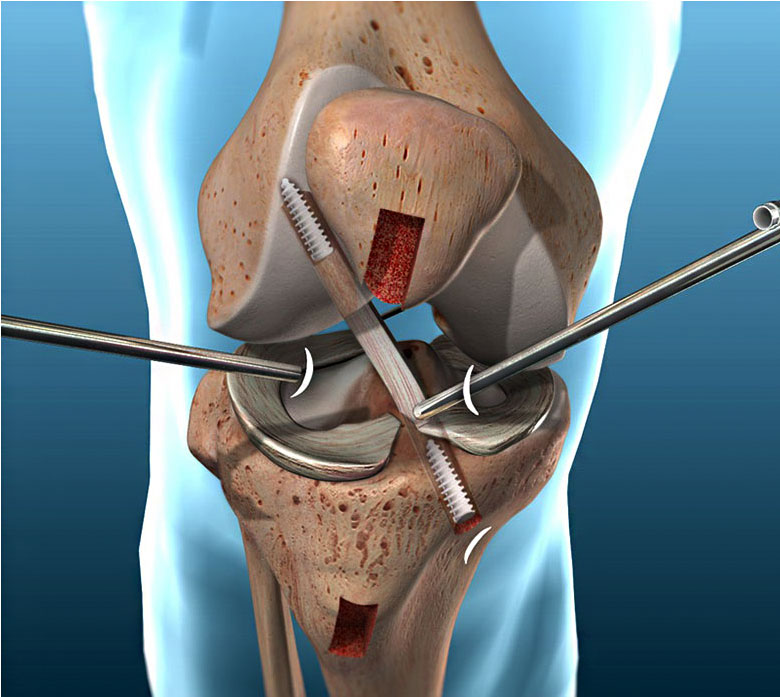
What is exactly done during the procedure?
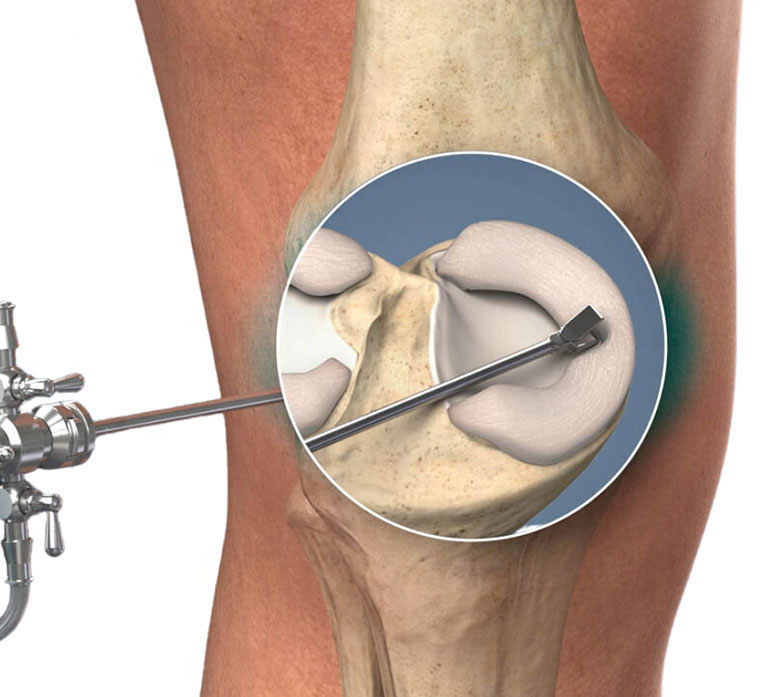
- Trimming or repairing torn meniscus
- Removing/ smoothing or repairing damaged cartilage
- Repairing or removing ligaments or tendons if necessary.
- Debriding (cleaning) the joint of damaged tissue or loose fragments.
Recovery
Recovery from knee arthroscopy is faster compared to traditional open surgery. Most patients can go home the same day, and they may need physical therapy for several weeks to regain strength and mobility.
ACL Reconstruction
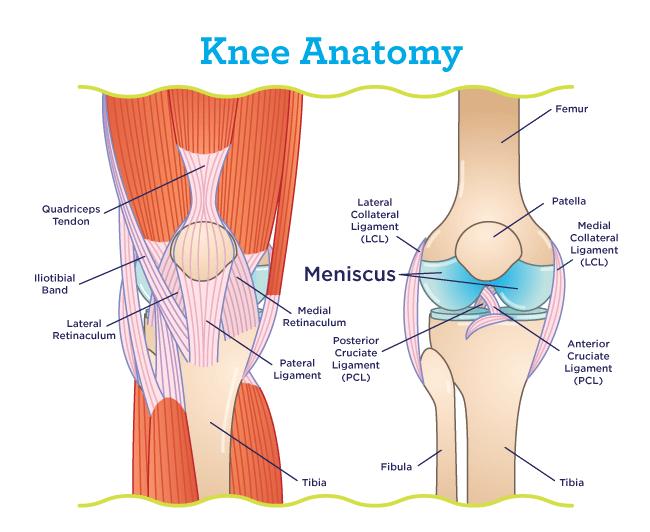
Your knee is a hinge joint where the end of the thigh bone (femur) meets the beginning of the large bone in your lower leg (tibia). A healthy knee has smooth cartilage that covers the ends of the femur and tibia. The smooth cartilage lets the surfaces of the two bones glide smoothly as you bend your knee. The muscles and ligaments around the knee joint support your weight and help move the joint smoothly so you can walk without pain.
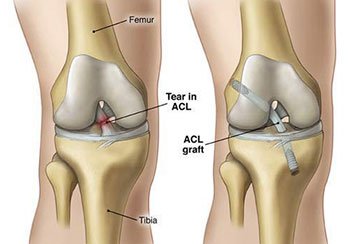
The Anterior Cruciate Ligament (ACL) is located in the center of the knee joint where it runs from the backside of the femur (thighbone) to connect to the front of the tibia (shinbone).
When Surgery Might Not Be Necessary:
1. Partial ACL Tears: If the ACL is partially torn but still provides enough stability to the
knee, some people may opt for non-surgical treatment. This typically includes physical
therapy to strengthen the muscles around the knee and improve stability.
2. Low Activity Levels: If you don't engage in high-demand sports or activities that require
quick directional changes (like basketball, soccer, or skiing), non-surgical options might
be enough. Many people can live a functional life with a torn ACL by focusing on
strengthening the knee and avoiding activities that could further damage the joint.
3. Older or Less Active Individuals: For people who are older or less physically active,
surgery may not be necessary. Non-surgical management (physical therapy, bracing,
and lifestyle adjustments) can be effective for managing the injury and maintaining knee
function.
When Surgery Is Often Recommended:
1. Complete ACL Tear: If the ACL is completely torn, surgery is often recommended,
especially for younger individuals or athletes, because the ligament cannot heal on its
own.
2. Instability: If the knee is unstable and "gives way" frequently, this can cause further
damage to the knee joint, leading to cartilage or meniscus injuries. Surgery helps restore
knee stability.
3. Active Athletes: Athletes or individuals who participate in sports that involve pivoting,
cutting, or jumping often benefit from surgery because the ACL is critical for knee
stability during these movements. A torn ACL can severely limit performance and
increase the risk of further injuries.
4. Younger Individuals: Young people with active lifestyles or who play sports are more
likely to undergo ACL surgery. This is because their active demands require a stable
knee, and non-surgical treatment alone may not provide the same level of functionality in
the long term.
For a complete tear of the ACL, reconstruction surgery is generally scheduled between 3 to 6 weeks after the injury occurs. This allows inflammation in the area to subside and allows time for physical therapy sessions to focus on restoring normal knee flexion and extension. If surgery is performed too early and in patients with limited knee range of motion, patients may develop a profound scarring response called arthrofibrosis, which leads to stiffness of the knee joint. Delaying surgery beyond three months increases the risk of developing irreparable cartilage damage or meniscus injuries because of continual instability in the knee.
Orthopedic surgeons gauge the appropriate timing of reconstruction surgery based on:
- Whether there are other injuries present that need to be treated first
- The physical appearance of the knee (how much swelling is present)
- The patient’s level of knee pain
- The patient's range of motion and quality of muscle control when flexing (bending) or extending (straightening) the leg
Some evidence suggests that delaying ACL reconstruction surgery for six months or longer after injury can not only increase the risk of sustaining a meniscus tear or cartilage injury, but also lead to increased risk of the need for a future ACL revision surgery.
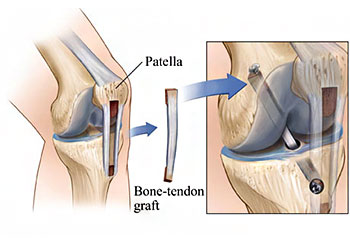
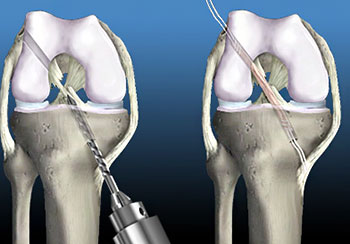
In ACL reconstruction surgery, a new ACL is made from a graft of replacement tissue from one of two sources:
- A portion of the patient's own iliotibial band, hamstring, quadriceps or patellar tendon
- An allograft (tissue from a human organ donor)
The type of graft used for each patient is determined on a case-by-case basis, however allograft tissue is not advised for young patients due to the significantly higher risk of reinjury and graft failure.
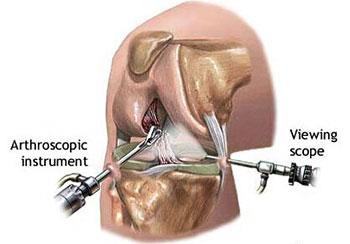
ACL reconstruction surgery is performed using minimally invasive arthroscopic techniques, in which a combination of fiber optics, small incisions and small instruments are used. A somewhat larger incision is needed, however, to obtain the tissue graft. ACL reconstruction is an outpatient (ambulatory) procedure, in which patients can go home on the same day as their surgery.
Initial Recovery: The patient is usually discharged the same day or after a short stay in the hospital. They may need crutches for a few weeks and are often advised to rest and elevate the knee to reduce swelling
Physical Therapy:Rehabilitation is a critical part of the recovery process. It helpsrestore strength, range of motion, and stability in the knee. Therapy may begin as soon as the patient is able, focusing initially on gentle exercises and progressing to more intense activities as healing continues.
Return to Sports:Athletes can generally return to sports 6-9 months after surgery, but the recovery timeline can vary depending on individual progress and rehabilitation. It’s important to ensure the knee is fully healed and stable before resuming high-impact activities.
Meniscus Surgery
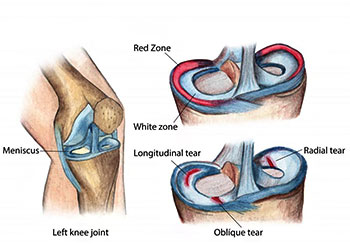
The meniscus is a soft, rubber-like C-shaped cushion in between the bones of the knee. There are two of them – one on the inner side (medial meniscus) and one on the outer side (lateral meniscus). These structures act as shock absorbers. They share the load on the knee and protect the cartilage cap over the knee bones. There are two problems which occur in menisci – one, that it degenerates (becomes weak) with age, and the other that it tears due to injury.
A degeneration in the meniscus causes pain, having become softer it often breaks with minimum injury. A typical meniscus tear occurs in young adults, as a result of twisting injury.
You’ll need some or all of the following tests before your meniscus surgery:
- Physical exam
- Blood tests
- EKG
- Chest X-ray
- Knee X-ray
- MRI
Tell your provider and surgeon what medications and over-the-counter (OTC) or herbal supplements you take. You may have to stop taking some prescriptions or supplements before your surgery.
Your surgeon will tell you when you should fast (stop eating and drinking) the day before your surgery. Most people need to fast for 12 hours before their surgery.
Plan to arrange transportation to and from your surgery. You won’t be able to drive yourself home after surgery, so make sure someone’s available to pick you up.
The day of your surgery, an anesthesiologist will give you anesthesia to numb your body and make sure you don’t feel pain during the procedure. They’ll give you either general anesthesia that puts you to sleep or regional anesthesia that numbs you from the waist down. If you need regional anesthesia, your anesthesiologist will also give you a sedative to relax you.
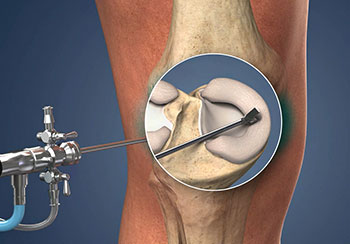
Meniscus surgery is usually done with a minimally invasive knee arthroscopy. Your surgeon will make a few cuts (incisions) in the skin around your knee. They’ll insert tiny tools and a small camera into your knee joint to treat the meniscus tear. There are three types of meniscus surgery:
- Meniscus repair
- Partial meniscectomy
- Meniscus replacement
Meniscus repair: A meniscus repair is just what it sounds like — your surgeon will repair the tear and any other damage in your meniscus. They’ll stitch (suture) the tear together so your meniscus heals back into one piece. Your body will absorb the sutures as the tear heals.
Partial meniscectomy: A “partial meniscectomy” is the medical term for removing the damaged part of your meniscus. Your surgeon will trim the damaged cartilage away from your meniscus and leave healthy tissue in place. Meniscectomy is a good option for more severe tears. Higher-grade meniscus tears usually are too severe to heal back together completely, even with a repair.
Meniscus replacement: Meniscus replacement (meniscus transplantation) is much less common than the other two types. It’s usually only a good option for people younger than 50 who have knee arthritis or a severely torn meniscus. Your surgeon will replace your meniscus with an allograft (a meniscus from a human donor).
Meniscus surgery usually takes around an hour. It might take a little more or less time depending on which type of surgery you need, the severity of the tear and if you have any other injuries (like knee ligament tears) that need treatment, too.
Meniscus surgery is usually an outpatient procedure. That means you can go home the same day. Your surgery team will monitor you in a recovery room while the anesthesia wears off. When it’s safe for you to go home, you’ll need someone to drive you.