Joint Preservation
If you have recurring or chronic joint pain, you may think joint replacement surgery is your only option for relief. However, you may want to explore several less invasive options first to help maintain mobility as you age. With millions of people wanting to stay active into their 60s, 70s and beyond, much recent research has focused on joint health and replacement technology.
Experiencing joint pain doesn’t automatically mean that you should have a joint replacement!
Joint replacement surgery is generally performed for late stages of degenerative arthritis (also called osteoarthritis), after other options have failed. Most causes for joint pain including knee, hip, shoulder and ankle can be treated with far less invasive options.
What is joint preservation — and when is it the best option?
The goal of preservation is to prevent injury, reduce inflammation and preserve cartilage, Dr. Miniaci says. These factors figure in when your physician weighs your options:
Age: Preservation techniques often are more successful the younger you are.
Weight: The more you weigh, the greater stress and demand is placed on your joints. Every pound you lose relieves three to five pounds of pressure on the hip, knee or ankle. Losing weight is the best thing you can do for an arthritic joint.
Muscle strength and conditioning: Muscles provide power to movement. They also serve as shock absorbers, protecting your joints. Maintaining or restoring muscle strength and flexibility reduces joint stress and pain.
Severity: Your doctor may sometimes manage small areas of cartilage thinning or erosion with minimally invasive procedures. However, if the cartilage is almost all gone — leaving bone touching bone, or if the bone underneath the cartilage is deteriorating, surgery is sometimes the best option although some injections can still help in those situations.
Location: Many joint preservation techniques focus on the knees. But there are an increasing number of alternatives to hip and shoulder replacement as well.
Non-surgical options for treating joint pain
Injections: Injections of hyaluronic acid or corticosteroids can reduce inflammation in many patients in the lining of the joints. These treatments can work in most joints and have been well-studied and results are mixed. But not all insurance carriers will cover these injections.
Platelet-rich plasma: Your blood contains platelets — hundreds of thousands of platelets are present in every milliliter of blood. These contain chemicals that can stimulate tissue repair, reduce inflammation and stimulate your own cells in the healing response. Because of this, many clinicians have begun using injections of concentrated plasma which includes platelets from blood to treat inflamed or injured tendons, ligaments, muscle and joints.
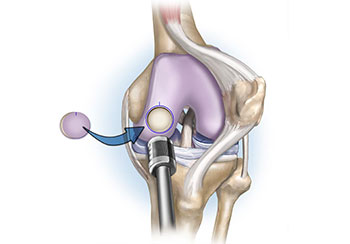
Cartilage transplant: In this technique, your treatment team will grow, transplant or use a cartilage replacement and place it in the damaged space. They can also stimulate the bone in your joint to increase cartilage growth. Not one technique is the proven best and much work needs to be done.
High Tibial Osteotomy, Distal Femur Osteotomy: These are alignment correction surgeries. They are performed when your cartilage is normal and the main culprit to your issues is found to be your alignment (if your legs are crooked).
A very small cut/ microfracture is created in your bones (tibia or femur), your legs are made straight again and plates/ screws are applied to hold the correction. Weight bearing is allowed after 6 weeks. Complete recovery usually takes 3 to 6 months. The biggest advantage is, you may never need a joint replacement in your life. Your knees are yours.
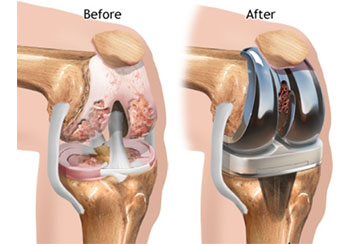
The benefits of full joint replacement
If you’ve unsuccessfully attempted conservative treatment or if damage to the cartilage or bone is beyond repair, remember that joint replacement is proven to be safe and highly effective in the right patient. Dr. Miniaci says this is still often your best option. Newer techniques in the hip and shoulder as well as knee can give patients excellent pain relief and improved function. However, there are always potential risks and complications with surgery.
Talk with your doctor about the best options and long-term strategies for you and understand what’s available for your specific problem. Preserving your joints and your activities and lifestyle is the basis for a partnership that is best for you.
What are the most common parts of the body injured?
➣ Achilles tendon: The Achilles tendon is a thick cord that connects the back of your lower leg (calf) to your heel. It helps you walk. But the tendon can become swollen, inflamed and stiff. It can even tear. This is called Achilles tendinitis or Achilles tendon rupture.
➣ Ankle: Your leg and foot join together at your ankle. It contains three joints, as well as several bones, cartilage, ligaments, muscles and tendons. Ankle pain is often caused by a sprained ankle. ATFL (anterior talo-fibular ligament) is the one which is most commonly damaged.
➣ Elbow: Your elbow is the joint that acts as a hinge between your upper and lower arm. People often experience pain in their elbow from repeat motions and overuse (eg: tennis elbow and golfer’s elbow)
➣ Knee: Your knee is a complex joint that acts as a hinge between your thigh and lower leg. It contains bones, cartilage, ligaments and tendons. Knee pain can be caused by jumper’s knee or runner’s knee. Other common injuries include meniscus tear and anterior cruciate ligament (ACL) tear.
➣ Shoulder: Your shoulder connects your upper arm to the trunk of your body. It contains your rotator cuff, a group of muscles and tendons that keep the upper arm in your shoulder socket. Rotator cuff tendinitis and rotator cuff tears are common sports injuries.